|
|
SMILE LASIK
|
 Only Place for Flapless & Bladeless LASIK in Rajasthan
Who is ReLEx SMILE most suitable for?
Only Place for Flapless & Bladeless LASIK in Rajasthan
Who is ReLEx SMILE most suitable for?
 ReLEx SMILE is most suitable for short-sighted people, especially those who may have been told they were not candidates for laser eye surgery because of thin corneas, dry eyes, or contact lens intolerance.
ReLEx SMILE is most suitable for short-sighted people, especially those who may have been told they were not candidates for laser eye surgery because of thin corneas, dry eyes, or contact lens intolerance.
Differences between ReLEx and LASIK
 ReLEx represents the beginning of a new era in refractive surgery, on the grounds of its significant advantages in terms of the patient’s comfort. Because there is no need to pass from one instrument to another – as in the LASIK procedure – there is no need for the patient to change their position. This is the main reason why the procedure only takes a few minutes.
The ReLEx SMILE procedure: How it works
ReLEx represents the beginning of a new era in refractive surgery, on the grounds of its significant advantages in terms of the patient’s comfort. Because there is no need to pass from one instrument to another – as in the LASIK procedure – there is no need for the patient to change their position. This is the main reason why the procedure only takes a few minutes.
The ReLEx SMILE procedure: How it works
ReLEx SMILE (often known simply as SMILE, which stands for Small Incision Lenticule Extraction) is, by its less invasive nature, a method that allows correction of even higher myopic prescriptions than previously treatable by standard LASIK laser eye surgery.
During the procedure, eye anaesthetic drops are used to completely numb the eye, and the state-of-the-art Carl Zeiss VisuMax laser places a series of pulses in the centre of the cornea with extraordinary 3D placement accuracy. These pulses form bubbles that are less than 1/100th the width of a human hair, and which outline the tissue that needs to be removed to effectively change the shape of the cornea.
The laser then creates a tiny connecting tunnel through which the surgeon draws out this tissue.
With ReLEx SMILE, no flap is created, so the healing time is faster than conventional LASIK. The procedure takes a matter of minutes, and the vision is 80% better instantly and reaches 100% within a few days (according to trials conducted on over 1,000 patients between the UK, Germany, France and Denmark).
ReLEx® (Refractive LEnticule Extraction) SMILE (SMall Incision Lenticule Extaction) is the very latest laser eye surgery techniques used to treat short-sightedness, with or without astigmatism. This treatment is available in only a few laser eye surgery clinics worldwide. Patients get all the benefits of LASIK - rapid healing and very little discomfort - but now without having a corneal flap.
No ablation No flap
 ReLEx® SMILE uses state-of-the-art femtosecond technology to create a high-precision lenticule (thin circular disc of tissue) that is removed through a small incision in an intact cornea. It relaces the roughly 20 mm side cut of LASIK to a small incision of less than 4 mm.
Your eye is anaesthetised with eye drops and a lid speculum is gently positioned to prevent you from accidently blinking. The whole treatment process is then undertaken using our Visumax femtosecond laser as a single step.
The whole treatment usually takes between 10 to 15 minutes, the actual laser is in operation for only a tiny fraction of this time, and after a quick post operative check by your surgeon, you are free to go. The recovery from ReLEx is generally quite comfortable (similar to Lasik) and the visual reasonably quick. You should have hazy but navigational vision when you get up off the couch but it is always wise to take a few days off after your surgery and some patients may prefer to pencil in a little longer off work in case you need it. Visual recovery wih ReLExSmILE is generall a little slower than Lasik. Follow up appointments are generally the next day, then between 7 and 14 days, then 1-3 and then 6 months later. We tend to judge the success ReLEx SMILE treatment at about 3 months but we will keep a check on your progress for at least 9 to 12 months.
SMILE: A Significant Milestone in Lasik
ReLEx® SMILE uses state-of-the-art femtosecond technology to create a high-precision lenticule (thin circular disc of tissue) that is removed through a small incision in an intact cornea. It relaces the roughly 20 mm side cut of LASIK to a small incision of less than 4 mm.
Your eye is anaesthetised with eye drops and a lid speculum is gently positioned to prevent you from accidently blinking. The whole treatment process is then undertaken using our Visumax femtosecond laser as a single step.
The whole treatment usually takes between 10 to 15 minutes, the actual laser is in operation for only a tiny fraction of this time, and after a quick post operative check by your surgeon, you are free to go. The recovery from ReLEx is generally quite comfortable (similar to Lasik) and the visual reasonably quick. You should have hazy but navigational vision when you get up off the couch but it is always wise to take a few days off after your surgery and some patients may prefer to pencil in a little longer off work in case you need it. Visual recovery wih ReLExSmILE is generall a little slower than Lasik. Follow up appointments are generally the next day, then between 7 and 14 days, then 1-3 and then 6 months later. We tend to judge the success ReLEx SMILE treatment at about 3 months but we will keep a check on your progress for at least 9 to 12 months.
SMILE: A Significant Milestone in Lasik
What is Femtosecond Technology: BASIC PRINCIPLES
How short is ultrashort? The definition of a femtosecond is 10-15 seconds (ie, one millionth of a billionth of a second). Putting that information into comprehensible terms, it takes 1.2 seconds for light to travel from the moon to an earthbound observer’s retinas. In 100 femtoseconds, light traverses 30 µm—around one-third the thickness of a human hair. During that time, laser pulses can carry energies of some nano- to microJoules, which leads to peak power equivalent to that produced at nuclear power plants (mega- to gigawatts). Most ophthalmologists are familiar with the linear absorption of light energy, which leads to the process known as photoablation that is produced by excimer lasers.
Femtosecond lasers produce a different tissue interaction, however, known as photodisruption (Figure 1). The application of many photons of laser energy at the same place and time leads to a nonlinear absorption of femtosecond laser energy. Due to the multiphoton effect, as well as the electron avalanche phenomenon, energy absorption by tissue eventually exceeds the threshold for optical breakdown. This process of photodisruption creates plasma. It also produces an acoustic shockwave, some thermal energy, and then a cavitation bubble, which expands at supersonic speed, slows down, and then implodes. A gas bubble subsequently forms that is composed of carbon dioxide, water, nitrogen, and other elements. The effect of photodisruption on tissue varies as infrared laser energy decreases from the level of micro- to nanoJoules. Nd:YAG lasers are used to produce posterior capsulotomies at milliJoule energies (10-nanosecond pulse duration). Femtosecond lasers can cut LASIK flaps at microJoule energy (approximately 930-femtosecond pulse duration), LASIK flaps almost without bubbles at 100 nanoJoules (200-femtosecond pulse duration), and chromosome cutting with femtoscissors at 1 nanoJoule (90-femtosecond pulse duration) with a lens that has a very high numerical aperture.
The threshold for optical breakdown (photodisruption) is inversely related to the laser’s intensity. The shorter the pulse’s duration and the smaller the diameter (and volume) of the spot, the lower the energy needed for photodisruption. A lens with a higher numerical aperture will create a more focal laser spot in terms of its diameter and volume, which enhances the depth accuracy and overall precision of the lamellar cut. This strategy of a higher numerical aperture lens is employed by the Visumax and Ziemer systems. Lower pulse energy is generally associated with fewer unwanted side effects, such as an opaque bubble layer, collateral thermal damage, and possibly diffuse lamellar keratitis as well as transient light sensitivity.
 Figure 1. The course of a photodisruptive process is shown. Due to multiphoton absorption in the focus of the laser beam, plasma develops (A).Depending on the laser parameter, the diameter varies between 0.5 µm to several micrometers. The expanding plasma drives as a shock wave, which transforms after a few microns to an acoustic transient (B).In addition to the shock wave’s generation, the expanding plasma has pushed the surrounding medium away from its center, which results in a cavitation bubble (C).The maximum diameter of the cavitation bubble can reach 10 to 100 µm .Its lifetime is only a few microseconds. After the collapse of the cavitation bubble,a gas bubble is left behind, containing carbon dioxide and other gas molecules (D).
There are two basic paradigms in the photodisruptive process. One employs high-energy (microJoule) pulses and a low-frequency pulse engine (kHz). The other relies on low-energy (nanoJoule), high-frequency (MHz) pulses. The VisuMax relies on low-energy (nanoJoule), high-frequency (MHz) pulses. Lower-energy pulses and smaller spot sizes and volumes require the use of substantially more spots placed closer together, because the plasma itself is the primary driver of the cutting process. To deliver this many spots in a reasonable timeframe requires a very-high-frequency engine.
Figure 1. The course of a photodisruptive process is shown. Due to multiphoton absorption in the focus of the laser beam, plasma develops (A).Depending on the laser parameter, the diameter varies between 0.5 µm to several micrometers. The expanding plasma drives as a shock wave, which transforms after a few microns to an acoustic transient (B).In addition to the shock wave’s generation, the expanding plasma has pushed the surrounding medium away from its center, which results in a cavitation bubble (C).The maximum diameter of the cavitation bubble can reach 10 to 100 µm .Its lifetime is only a few microseconds. After the collapse of the cavitation bubble,a gas bubble is left behind, containing carbon dioxide and other gas molecules (D).
There are two basic paradigms in the photodisruptive process. One employs high-energy (microJoule) pulses and a low-frequency pulse engine (kHz). The other relies on low-energy (nanoJoule), high-frequency (MHz) pulses. The VisuMax relies on low-energy (nanoJoule), high-frequency (MHz) pulses. Lower-energy pulses and smaller spot sizes and volumes require the use of substantially more spots placed closer together, because the plasma itself is the primary driver of the cutting process. To deliver this many spots in a reasonable timeframe requires a very-high-frequency engine.
 Figure 2 Higher pulse energy (A) allows the use of greater spacing between spots, because the cutting process is driven primarily by expanding cavitation and residual gas bubbles. Lower pulse energy (B) and smaller spot size and volume require substantially more spots with tighter spacing and greater overlap, as the cutting process here is driven primarily by the plasma itself. To deliver this many spots in a reasonable time frame requires a very-high-frequency engine (VISUMAX).
Femto SMILE
lenticular extraction with the femtosecond laser is the real all LASER procedure. This involves making two lamellar cuts with a femtosecond laser to create an intrastromal lenticle of defined shape, which the surgeon removes. We have used the VisuMax in this fashion for myopic treatments. They create a huge optical zone and a slightly prolate cornea without any need for the excimer laser ablation of tissue.
Figure 2 Higher pulse energy (A) allows the use of greater spacing between spots, because the cutting process is driven primarily by expanding cavitation and residual gas bubbles. Lower pulse energy (B) and smaller spot size and volume require substantially more spots with tighter spacing and greater overlap, as the cutting process here is driven primarily by the plasma itself. To deliver this many spots in a reasonable time frame requires a very-high-frequency engine (VISUMAX).
Femto SMILE
lenticular extraction with the femtosecond laser is the real all LASER procedure. This involves making two lamellar cuts with a femtosecond laser to create an intrastromal lenticle of defined shape, which the surgeon removes. We have used the VisuMax in this fashion for myopic treatments. They create a huge optical zone and a slightly prolate cornea without any need for the excimer laser ablation of tissue.
 Figure 3. Incision geometry of the ReLEx SMILE procedure. The lenticule cut is performed (the underside of the lenticule), followed by the lenticule sidecuts. Next, the cap interface is created (the upper side of the lenticule), and finally a 2- to 3-mm small incision is created super-temporally. The lenticule interfaces are separated using a flap separator, and the lenticule is extracted manually, all via the small incision.
Figure 3. Incision geometry of the ReLEx SMILE procedure. The lenticule cut is performed (the underside of the lenticule), followed by the lenticule sidecuts. Next, the cap interface is created (the upper side of the lenticule), and finally a 2- to 3-mm small incision is created super-temporally. The lenticule interfaces are separated using a flap separator, and the lenticule is extracted manually, all via the small incision.

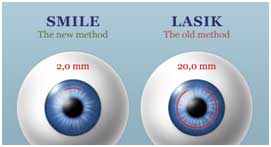 Fig incision size in Smile is reduced to <4 mm from 20 mm in Lasik.
Fig incision size in Smile is reduced to <4 mm from 20 mm in Lasik.
 Figure 4. Diagram of the steps of the refractive procedure using the femtosecond laser system. A and C: View of a cross-section through the cornea. B and D: Top view of the cornea. Surface 1 is the posterior surface of the lenticule. Surface 2 is the lenticule side cut. Surface 3 is the anterior surface of the lenticule. Surface 4 is the side-cut incision. C and D show the lenticule being extracted from the cornea.
Figure 4. Diagram of the steps of the refractive procedure using the femtosecond laser system. A and C: View of a cross-section through the cornea. B and D: Top view of the cornea. Surface 1 is the posterior surface of the lenticule. Surface 2 is the lenticule side cut. Surface 3 is the anterior surface of the lenticule. Surface 4 is the side-cut incision. C and D show the lenticule being extracted from the cornea.
 Figure 5. This is a diagrammatic demonstration showing the difference in strength of the remaining stroma after PRK, LASIK, and ReLEx SMILE. These diagrams show that the strength of the stroma remaining after ReLEx SMILE is greater than the equivalent treatment as both PRK and LASIK. The fact that Bowman's layer remains intact will also provide added strength. Finally, the two diagrams for ReLEx SMILE show the even greater strength if the lenticule is removed from deeper within the stroma.
Source (all): Dan Z. Reinstein, M.D.
Conclusions: According to our experience, SMILE is the way ahead in Femto technology which is effective and safe procedure for both patients and doctors for correction of myopia and myopia with astigmatism.
Figure 5. This is a diagrammatic demonstration showing the difference in strength of the remaining stroma after PRK, LASIK, and ReLEx SMILE. These diagrams show that the strength of the stroma remaining after ReLEx SMILE is greater than the equivalent treatment as both PRK and LASIK. The fact that Bowman's layer remains intact will also provide added strength. Finally, the two diagrams for ReLEx SMILE show the even greater strength if the lenticule is removed from deeper within the stroma.
Source (all): Dan Z. Reinstein, M.D.
Conclusions: According to our experience, SMILE is the way ahead in Femto technology which is effective and safe procedure for both patients and doctors for correction of myopia and myopia with astigmatism.
|
|
|
|
